
Whole-body magnetic resonance imaging (WB-MRI), which involves imaging of the head, neck, chest, abdomen, pelvis, and bones, has emerged as a valuable tool for cancer detection, particularly in the pediatric population with cancer predisposition syndrome. WB-MRI provides excellent soft tissue contrast resolution and is free from ionizing radiation [1, 2]. In a prospective observational study on patients with Li-Fraumeni syndrome, implementation of WB-MRI in the surveillance group provided early tumor detection and improved long-term survival (5 year overall survival rates, 88.8% vs. 59.6%), compared with non-surveillance group [3].
Recent advances in WB-MRI techniques have enabled imaging procedures to be completed within 60 to 90 min, depending on the sequence components [4–6]. The increasing popularity of WB-MRI as a screening tool for individuals who self refer themselves for wellness checkups has resulted in the widespread utilization of the technique worldwide [5, 7]. However, a review of 12 studies revealed that abnormal findings requiring further evaluation were detected in up to 30% of 3331 asymptomatic individuals screened using WB-MRI [5]. A classification of these findings based on cancer risk is crucial to facilitate effective post screening
consultation and management.
In 2021, an international multidisciplinary expert panel proposed a set of guidelines, known as the Oncologically Relevant Findings Reporting and Data System (ONCORADS) guidelines, to establish a standardized approach for the acquisition and reporting of WB-MRI results for cancer screening [8]. Specifically, the ONCO-RADS guidelines employs a 5-category scoring system to evaluate abnormal findings based on the likelihood of cancer in multiple body regions. The standardized data collection method aims to reduce the variability of WB-MRI interpretations and direct risk-based management. However, the application of ONCO-RADS requires empirical validation. Thus, the present study assessed the reliability of ONCO-RADS and explored the prevalence rates of cancer in asymptomatic individuals undergoing WB-MRI according to ONCO-RADS classifications.
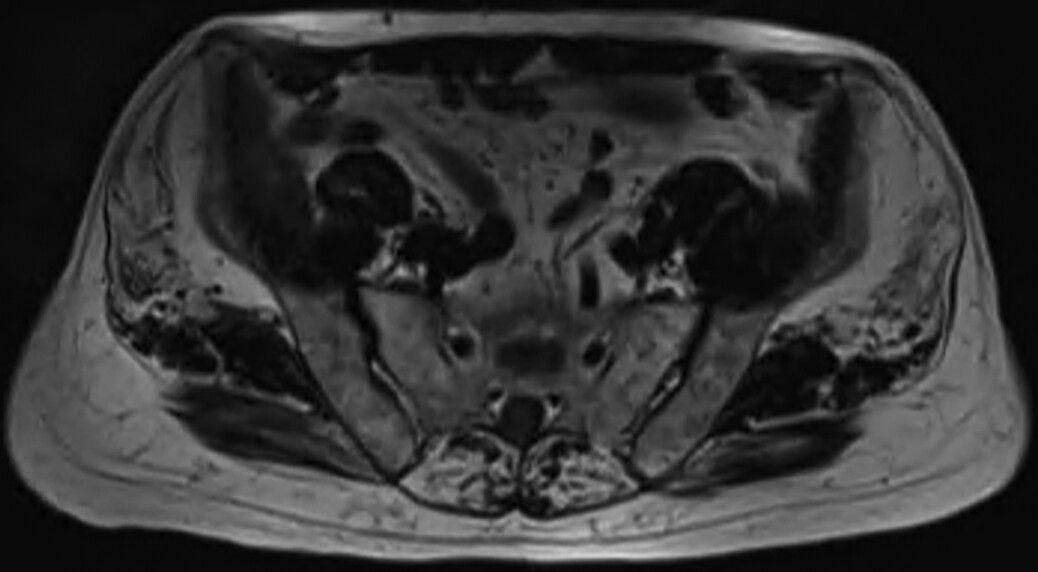
Participants and study design The requirement for informed consent was waived because of the retrospective nature of this study. The STROBE reporting guidelines were implemented. From September 2017 to March 2022, 2203 self-referred individuals participated in a WB-MRI screening program at our institute. The WB-MRI screening program involves WB-MRI examinations, laboratory tests, and other optional imaging studies, including ultrasound and lowdose chest CT scan. Participants completed a questionnaire to collect data on current symptoms, personal medical history, surgical history, and family history of cancer. Individuals were included if they were aged ≥ 18 years, asymptomatic, and had been cancer-free for ≥ 5 years. Individuals with significant clinical symptoms (n = 21) or those who had not been cancer-free for ≥ 5 years (n = 118) were excluded. In total, 2064 participants were included for analysis. WB-MRI examinations and follow-up strategy MRI was acquired on a 3-T system with a 70-cm bore (Magnetom Skyra; Siemens Healthcare, Erlangen, Germany). The sequence components for WB-MRI at our institute and the recommendation of ONCO-RADS are summarized in Table 1 [8]. In brief, T2-weighted images were acquired for all regions, with a slight difference in the imaging techniques according to the region.
Regional multisequence oncologic MRI, including DWI, was performed for the brain, abdomen, and pelvis. After the administration of 0.1 mmol/kg gadolinium-based contrast agent (Gadovist, Shering, Berlin, Germany),
dynamic T1 gradient echo images with fat saturation were acquired for the abdomen, followed by T1-weighted images for the other regions. The average empirical WBMRI examination time was 68 min. No severe adverse
reactions to the contrast agent were reported. Adjunct ultrasound examinations of the thyroid and whole abdomen were performed in all participants. Board-certified radiologists experienced in MRI interpretation reviewed all images and provided participants with a summary of the findings on site, along with a formal report in 7 days. Depending on the findings, specialty referrals for further investigations at our institute were arranged.