Giuseppe Petralia, MD • Dow-Mu Koh, MD • Raj Attariwala, MD, PhD • Joseph J. Busch, MD • Ros Eeles, MD • David Karow, MD, PhD • Gladys G. Lo, MD • Christina Messiou, MD • Evis Sala, MD, PhD • Hebert A. Vargas, MD • Fabio Zugni, MD • Anwar R. Padhani, MD
From the Precision Imaging and Research Unit, Department of Medical Imaging and Radiation Sciences (G.P.), and Department of Radiology (F.Z.), IEO European Institute of Oncology IRCCS, Via Giuseppe Ripamonti 435, 20141 Milan, Italy; Department of Oncology and Hemato-Oncology, University of Milan, Italy (G.P.); Department of Radiology, Royal Marsden Hospital and Institute of Cancer Research, Sutton, England (D.M.K., C.M.); AIM Medical Imaging, Vancouver, Canada (R.A.); Busch Center, Alpharetta, Ga (J.J.B.); The Institute of Cancer Research and Royal Marsden NHS Foundation Trust, London, England (R.E.); Human Longevity, San Diego, Calif (D.K.); Department of Diagnostic & Interventional Radiology, Hong Kong Sanatorium & Hospital, Hong Kong (G.G.L.); Department of Radiology and Cancer Research, UK Cambridge Center, Cambridge, England (E.S.); Department of Radiology, Memorial Sloan-Kettering Cancer Center, New York, NY (H.A.V.); and Paul Strickland Scanner Centre, Northwood, England (A.R.P.). Received April 24, 2020; revision requested June 16; revision received November 5; accepted November 17. Address correspondence to G.P. (e-mail: giuseppe.petralia@ieo.it).
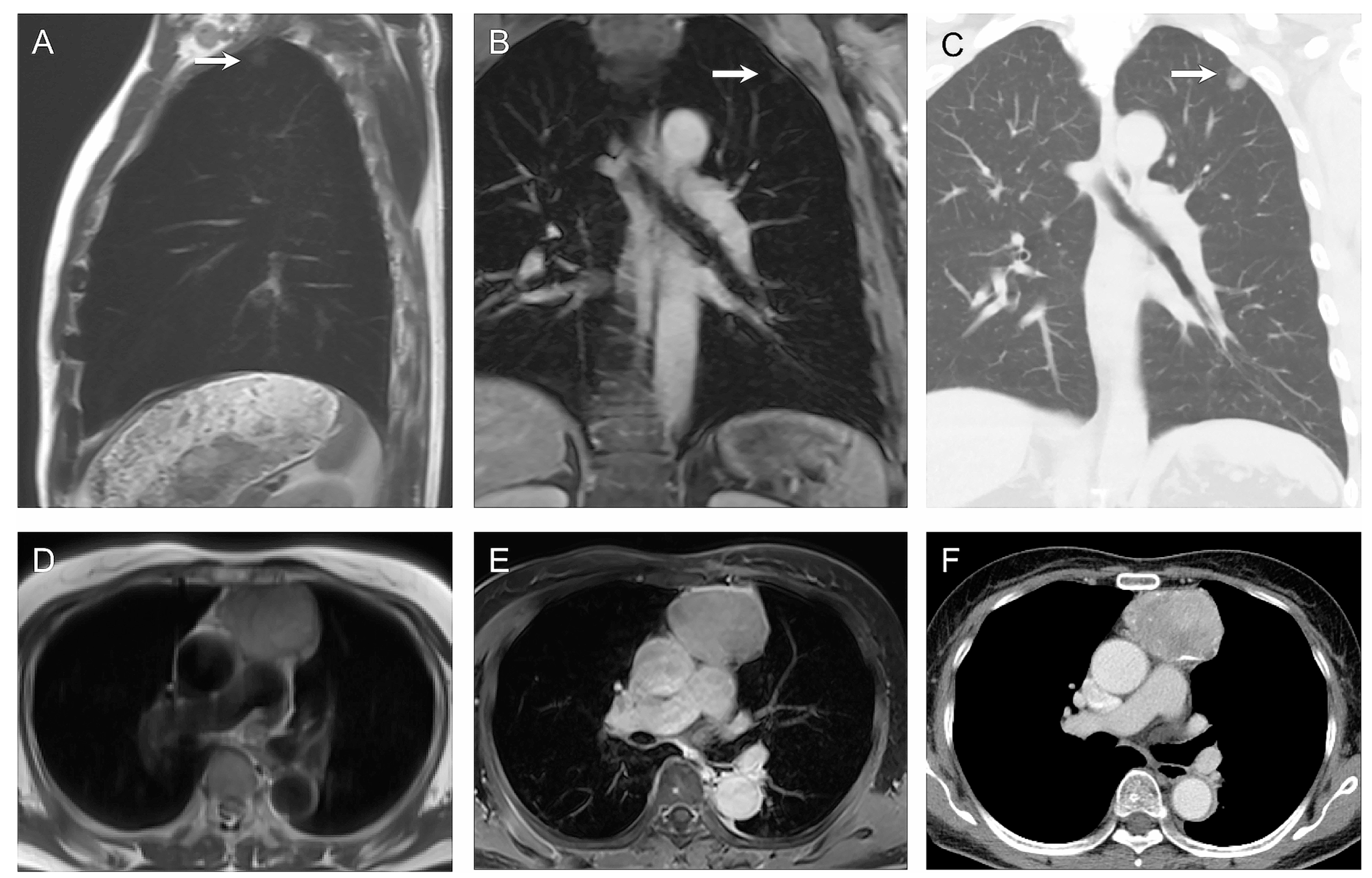
Several guidelines recommend the use of whole-body MRI for cancer screening in individuals with cancer predisposition syndromes. In Li-Fraumeni syndrome (LFS), wholebody MRI is indicated annually along with contrast-enhanced brain MRI (and breast MRI in adult women) as the techniques of choice for children and adults (1–4). Screening using whole-body MRI is also recommended for children and adults with hereditary paraganglioma and pheochromocytoma syndromes (5), whereas annual whole-body MRI from the age of 6 years is recommended in patients with constitutional mismatch repair deficiency syndrome (6) and from the age of 8 years in those with hereditary retinoblastoma (7). Whole-body MRI is also used in patients with neurofibromatosis for detecting the number, volume, and distribution of neurofibromas (8). The National Comprehensive Cancer Network recently suggested that there was a need to develop practice guidelines for introducing whole-body MRI as a method for detecting malignant peripheral nerve sheath tumors (9).
However, there is no recommendation on data acquisition methods for whole-body MRI when performed for cancer screening in individuals with cancer predisposition syndromes in terms of MRI protocols, including machine use, coil set-ups, imaging sequences, and anatomic coverage. Likewise, there is no consensus regarding the reading of screening whole-body MRI scans, nor on the reporting of examinations including how to deal with any abnormalities found.
This Oncologically Relevant Findings Reporting and Data System, or ONCO-RADS, consensus on whole-body MRI for cancer screening proposes standard protocols for higher-risk individuals.
Essentials N Whole-body MRI for cancer screening is recommended by international guidelines for cancer predisposition syndromes. N Standard and short acquisition protocols for whole-body MRI include anatomic and diffusion-weighted sequences, which can be completed in 50 minutes and 30 minutes, respectively. N Standardized acquisition protocols and structured reporting will support clinical deployment, training, and research in whole-body MRI for cancer screening.